H2: Unveiling the Surgical Revolution: How Augmented Reality is Transforming the Operating Room
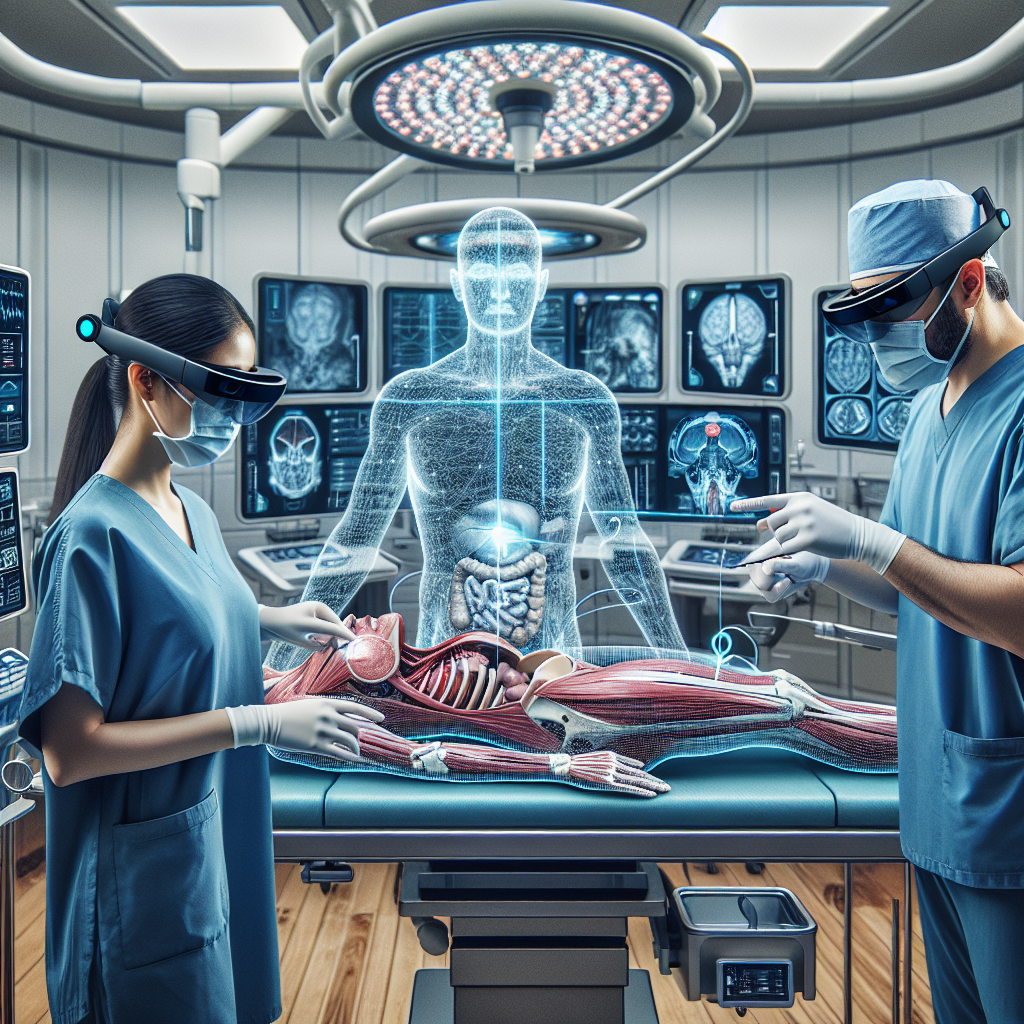
In the fast-paced world of medical advancements, one technology is poised to revolutionize the operating room: augmented reality (AR). Imagine a surgeon donning a pair of high-tech glasses that overlay digital information onto their field of vision, providing real-time guidance and enhancing their surgical precision. This futuristic concept is becoming a reality, with AR technology already making its way into surgical procedures around the world. In this article, we will explore the potential of augmented reality in surgery, its current applications, and the impact it may have on patient outcomes and the medical field as a whole.
Augmented reality, often associated with gaming and entertainment, is now finding its place in the medical realm. By seamlessly blending the physical and digital worlds, AR offers surgeons a new level of visualization and information that was previously unimaginable. From preoperative planning to intraoperative guidance, this technology has the potential to revolutionize surgical procedures and improve patient safety. We will delve into the various ways in which AR is being utilized, such as assisting in complex surgeries, training future surgeons, and even enabling remote collaboration between experts. Additionally, we will explore the challenges and ethical considerations that come with integrating this cutting-edge technology into the operating room.
Key Takeaways:
1. Augmented reality (AR) is revolutionizing the operating room by enhancing surgical precision and efficiency. Surgeons can overlay digital information onto the patient’s anatomy, providing real-time guidance and improving surgical outcomes.
2. AR technology enables surgeons to visualize complex anatomical structures, such as blood vessels and nerves, that are not visible to the naked eye. This allows for more precise surgical planning and reduces the risk of complications during procedures.
3. The use of AR in surgery has the potential to shorten operation times and decrease the need for invasive procedures. Surgeons can access vital patient information, such as medical images and lab results, directly through AR headsets, streamlining the surgical workflow.
4. Training and education in the field of surgery can greatly benefit from AR technology. Medical students and residents can practice surgical techniques in a virtual environment, gaining valuable experience before entering the operating room. This improves surgical skills and patient safety.
5. The future of surgery lies in the integration of AR with other advanced technologies, such as robotics and artificial intelligence. These synergistic approaches have the potential to revolutionize surgical procedures, making them safer, more precise, and accessible to a larger population.
The Integration of Augmented Reality in Surgical Training
One of the most exciting emerging trends in the future of surgery is the integration of augmented reality (AR) in surgical training. Traditionally, surgical trainees have relied on textbooks, lectures, and observing surgeries to learn essential skills. However, AR technology is revolutionizing the way surgeons are trained, providing a more immersive and interactive learning experience.
With AR, trainees can now visualize and practice surgeries in a virtual environment, allowing them to gain hands-on experience without the risks associated with real operations. Surgeons-in-training can wear AR headsets that overlay digital information onto their field of view, providing guidance and real-time feedback during surgical simulations.
This integration of AR in surgical training has several advantages. Firstly, it allows trainees to learn at their own pace, repeating procedures and refining their skills until they achieve proficiency. Secondly, AR technology can simulate complex surgeries that are rarely encountered, giving trainees exposure to a wider range of procedures. Lastly, AR can enhance the understanding of anatomical structures, making it easier for trainees to navigate and identify critical areas during surgery.
The implications of AR in surgical training are vast. As trainees become more proficient in virtual simulations, they will require less supervision during actual surgeries, potentially reducing the workload of experienced surgeons. Additionally, the use of AR can accelerate the learning curve for trainees, shortening the time required to become competent surgeons. Ultimately, the integration of AR in surgical training has the potential to improve patient outcomes by producing a new generation of highly skilled and confident surgeons.
Enhanced Surgical Visualization and Precision
Another significant trend in the future of surgery is the use of augmented reality to enhance surgical visualization and precision. Surgeons often rely on imaging techniques such as CT scans and MRI to plan and execute surgeries. However, these images are typically viewed on separate screens, requiring surgeons to mentally translate the information into the patient’s anatomy.
AR technology can seamlessly integrate these imaging techniques into the surgeon’s field of view, overlaying the patient’s internal structures onto their real-time vision. This allows surgeons to have a more comprehensive understanding of the patient’s anatomy during the operation, improving accuracy and reducing the risk of complications.
Furthermore, AR can provide real-time guidance during surgeries, highlighting critical structures, displaying vital signs, and even projecting virtual tools onto the surgeon’s hands. This augmented feedback can enhance precision and reduce errors, especially in complex procedures.
The implications of enhanced surgical visualization and precision are immense. Surgeons can perform surgeries with greater confidence and accuracy, resulting in improved patient outcomes and reduced complications. Additionally, the integration of AR in the operating room can potentially decrease the time required for surgeries, leading to shorter hospital stays and reduced healthcare costs.
Remote Surgery and Telemedicine
Remote surgery and telemedicine are emerging trends that have the potential to revolutionize the field of surgery. With the advancement of augmented reality, surgeons can now perform surgeries from a remote location, using robotic systems controlled through AR interfaces.
This technology enables expert surgeons to provide their expertise and perform surgeries in areas where specialized medical care is limited. Surgeons can guide local healthcare professionals through complex procedures, improving access to quality surgical care in underserved regions.
Furthermore, remote surgery can also be used in emergency situations, allowing surgeons to provide immediate assistance and expertise to patients in critical condition, regardless of their physical location.
Telemedicine, combined with AR technology, enables healthcare professionals to provide remote consultations and second opinions. Surgeons can use AR headsets to visualize patients’ conditions, review medical images, and collaborate with colleagues in real-time, even if they are miles apart.
The implications of remote surgery and telemedicine are far-reaching. Patients in remote areas can receive specialized surgical care without the need for extensive travel. Additionally, the ability to perform surgeries remotely can help alleviate the burden on healthcare systems by redistributing surgical expertise and reducing the strain on specialized surgical centers.
Overall, the integration of augmented reality in surgery holds immense potential for transforming the operating room. From revolutionizing surgical training to enhancing visualization and precision, and enabling remote surgery and telemedicine, AR technology is set to shape the future of surgery, improving patient outcomes, and expanding access to quality surgical care.
Controversial Aspect 1: Ethical Concerns
One of the most significant controversial aspects surrounding the use of augmented reality (AR) in surgery is the ethical concerns it raises. Critics argue that the integration of AR technology into the operating room may blur the line between human control and reliance on machines, potentially leading to a loss of surgical skills and expertise.
There is a fear that surgeons may become too reliant on AR systems, relying on the technology to guide their every move rather than relying on their own knowledge and experience. This raises concerns about the potential de-skilling of surgeons and the impact on patient safety.
On the other hand, proponents argue that AR technology can enhance surgical precision and reduce human error. By providing real-time visual guidance, AR systems can assist surgeons in identifying critical structures, improving surgical outcomes, and reducing the risk of complications. They argue that the technology should be seen as a tool that complements the surgeon’s skills rather than replacing them.
Controversial Aspect 2: Accessibility and Affordability
Another controversial aspect of the future of surgery with augmented reality is the issue of accessibility and affordability. AR technology is still relatively new and expensive, making it inaccessible to many healthcare institutions, particularly those in developing countries or with limited resources.
Critics argue that the adoption of AR systems in the operating room could exacerbate existing healthcare inequalities, as only well-funded institutions would be able to afford the technology. This could lead to a two-tiered healthcare system, where patients in wealthier areas have access to advanced AR-assisted surgeries, while those in less privileged areas do not.
Proponents, however, believe that as technology advances and becomes more widespread, the costs will decrease, making it more accessible to a wider range of healthcare institutions. They argue that the initial high cost should not overshadow the potential long-term benefits of improved surgical outcomes and reduced healthcare costs.
Controversial Aspect 3: Data Security and Privacy
Data security and privacy concerns are also raised when considering the integration of augmented reality in the operating room. AR systems rely on the collection and analysis of vast amounts of patient data, including medical images, patient records, and real-time surgical data. This raises concerns about the protection of patient information and the potential for data breaches.
Critics argue that the storage and transmission of sensitive patient data in AR systems could be vulnerable to hacking or unauthorized access, potentially compromising patient privacy and confidentiality. They also express concerns about the potential misuse of patient data for commercial purposes, such as targeted advertising or insurance discrimination.
Proponents acknowledge the valid concerns regarding data security and privacy but argue that robust measures can be implemented to ensure the protection of patient information. They emphasize the importance of secure data storage, encryption, and strict access controls to mitigate the risks. They also highlight the potential benefits of data collection and analysis in improving surgical techniques and patient outcomes through research and innovation.
Insight 1: Enhanced Visualization and Precision
One of the most significant impacts of augmented reality (AR) in the field of surgery is its ability to enhance visualization and precision during procedures. Traditional surgical techniques often rely on two-dimensional imaging techniques such as X-rays, CT scans, or MRI scans to guide surgeons. While these imaging methods provide valuable information, they lack the depth perception and real-time feedback that AR can offer.
By integrating AR technology into the operating room, surgeons can benefit from three-dimensional, high-resolution visualizations of the patient’s anatomy. This allows them to navigate complex anatomical structures with greater accuracy and make more informed decisions during surgery. AR overlays can provide real-time data, such as vital signs, lab results, and patient history, directly within the surgeon’s field of view, reducing the need to divert attention to external screens or monitors.
Moreover, AR can assist surgeons in preoperative planning by providing a virtual representation of the patient’s anatomy. Surgeons can simulate the procedure, evaluate different approaches, and anticipate potential challenges before stepping into the operating room. This technology not only enhances surgical precision but also reduces the risk of complications and improves patient outcomes.
Insight 2: Improved Training and Education
Augmented reality has the potential to revolutionize surgical training and education. Traditionally, surgeons-in-training rely on textbooks, lectures, and observing experienced surgeons to learn complex surgical techniques. While these methods are valuable, they often lack the immersive and hands-on experience necessary to develop surgical skills effectively.
AR can bridge this gap by providing trainees with realistic, interactive simulations of surgical procedures. By wearing AR headsets, trainees can visualize and practice surgical techniques on virtual patients, replicating the challenges and intricacies of real surgeries. This allows them to develop their skills in a safe and controlled environment, without the risk of harming actual patients.
Furthermore, AR can facilitate remote surgical mentoring and collaboration. Surgeons in training can connect with experienced surgeons from around the world in real-time, enabling them to receive guidance and feedback during procedures. This technology has the potential to democratize surgical education, making expertise more accessible to aspiring surgeons regardless of their geographical location.
Insight 3: Enhanced Patient-Doctor Communication and Informed Consent
Augmented reality can significantly improve patient-doctor communication and the informed consent process. Traditionally, surgeons use medical images and diagrams to explain surgical procedures to patients. However, these representations can be challenging for patients to understand, leading to confusion and anxiety.
With AR, surgeons can create interactive visualizations of the patient’s anatomy, allowing them to explain the procedure in a more intuitive and comprehensive manner. By wearing AR headsets, patients can see their own anatomy overlaid with virtual representations of the surgical plan, helping them visualize the potential outcomes and understand the risks and benefits more effectively. This enhanced communication can reduce patient anxiety, increase trust, and improve patient satisfaction.
AR can also play a crucial role in the informed consent process. By providing patients with a realistic visualization of the procedure, including potential complications and alternative treatment options, patients can make more informed decisions about their healthcare. This technology empowers patients to actively participate in their treatment plans, fostering a collaborative doctor-patient relationship.
The Benefits of Augmented Reality in Surgery
Augmented reality (AR) technology is revolutionizing the operating room by providing surgeons with real-time, interactive information during procedures. This technology overlays digital images onto the surgeon’s field of view, enhancing their perception and accuracy. One of the main benefits of AR in surgery is improved visualization. Surgeons can see important anatomical structures, such as blood vessels and nerves, that are otherwise hidden during traditional surgeries. This allows for more precise incisions and reduces the risk of complications.
AR also enables surgeons to plan and simulate procedures before entering the operating room. By using patient-specific imaging data, surgeons can create a 3D model of the patient’s anatomy and practice the surgery virtually. This helps them identify potential challenges and develop optimal surgical strategies. For example, in a case study conducted at Stanford University, surgeons used AR to plan a complex liver surgery. The virtual simulation allowed them to accurately predict the best approach and minimize the risk of complications during the actual surgery.
Improved Surgical Training and Education
Augmented reality has the potential to revolutionize surgical training and education. Traditionally, trainee surgeons learn by observing and assisting experienced surgeons during procedures. However, this approach has limitations, as trainees have limited access to the surgical field and often struggle to visualize complex anatomical structures.
With AR, trainee surgeons can wear a headset that overlays virtual images onto their view, providing a detailed and interactive learning experience. They can practice procedures, interact with virtual patients, and receive real-time feedback on their performance. This allows for a more immersive and hands-on training, leading to better surgical skills development. In fact, a study published in the Journal of Surgical Education found that surgical trainees who used AR technology showed significant improvement in their surgical skills compared to those who did not.
Enhanced Surgical Navigation and Precision
One of the key advantages of augmented reality in surgery is improved navigation and precision. Surgeons can use AR to visualize the patient’s internal anatomy in real-time, allowing for more accurate placement of surgical instruments and implants. This is particularly beneficial in minimally invasive procedures, where surgeons rely on small incisions and limited visibility.
By overlaying virtual images onto the surgeon’s view, AR provides guidance on the optimal trajectory and depth for surgical instruments. This helps reduce the risk of damaging surrounding tissues and improves the overall surgical outcome. For example, in a study published in the journal Neurosurgery, researchers used AR to guide the placement of screws during spinal fusion surgeries. The results showed that AR-assisted surgeries had higher accuracy rates and fewer complications compared to traditional techniques.
Improved Communication and Collaboration
Augmented reality technology facilitates improved communication and collaboration among surgical teams. During complex procedures, multiple healthcare professionals, including surgeons, anesthesiologists, and radiologists, need to work together seamlessly. However, communication challenges can arise due to differences in perspectives and limited visibility.
AR allows team members to share a common visual reference by overlaying virtual images onto their individual views. This enables better coordination and decision-making during surgeries. For example, in a case study conducted at the University of California, San Francisco, surgeons used AR to perform a complex brain tumor removal surgery. The technology allowed the surgical team to visualize the tumor’s location and plan the best approach collaboratively, resulting in a successful outcome.
Challenges and Limitations of Augmented Reality in Surgery
While augmented reality holds great promise in revolutionizing surgery, there are still challenges and limitations that need to be addressed. One of the main challenges is the integration of AR technology into existing surgical workflows. Surgeons need to adapt to wearing headsets and interacting with virtual images while performing procedures. This requires training and familiarization with the technology, which may take time.
Another limitation is the cost of implementing AR systems in operating rooms. The equipment, software, and maintenance expenses can be significant, making it difficult for smaller healthcare facilities to adopt the technology. Additionally, there are concerns regarding patient privacy and data security when using AR systems that require access to patient-specific imaging data.
Despite these challenges, the potential benefits of augmented reality in surgery are undeniable. As the technology continues to advance and become more accessible, we can expect to see its widespread adoption in operating rooms around the world. Augmented reality has the power to enhance surgical visualization, improve training, navigation, and collaboration, ultimately leading to better patient outcomes.
The Early Beginnings of Surgery
In order to understand the evolution of augmented reality in the operating room, it is important to first examine the early beginnings of surgery. Surgery has been practiced for thousands of years, with evidence of surgical procedures dating back to ancient civilizations such as Egypt and India. However, these early surgeries were often crude and lacked the sophisticated tools and techniques we have today.
During the Middle Ages, surgery was primarily performed by barber-surgeons, who were responsible for both cutting hair and performing surgical procedures. This period saw limited advancements in surgical techniques, with most surgeries being performed in unsanitary conditions and resulting in high mortality rates.
The Renaissance and the Birth of Modern Surgery
The Renaissance marked a turning point in the history of surgery. The invention of the printing press allowed for the dissemination of medical knowledge, leading to increased understanding of anatomy and surgical techniques. This period also saw the emergence of pioneering surgeons such as Ambroise Paré, who introduced new methods for treating wounds and developed innovative surgical instruments.
With the advent of anesthesia in the 19th century, surgery became less painful and more complex procedures could be performed. Surgeons began to specialize in specific areas, such as neurosurgery and orthopedic surgery, further advancing the field.
The of Laparoscopy
In the 20th century, laparoscopy revolutionized the field of surgery. This minimally invasive technique allowed surgeons to perform procedures through small incisions, reducing patient trauma and improving recovery times. Laparoscopy became widely adopted in the 1980s and 1990s, transforming surgeries such as gallbladder removal and appendectomies.
However, laparoscopy still had limitations. Surgeons had to rely on two-dimensional images displayed on a monitor, making depth perception and spatial awareness challenging. This led to the development of three-dimensional laparoscopy systems, which provided surgeons with a more realistic view of the surgical field.
The Emergence of Augmented Reality
Augmented reality (AR) technology started gaining traction in the early 2000s, with the development of wearable devices such as Google Glass. This technology superimposed digital information onto the user’s field of view, opening up new possibilities for various industries, including healthcare.
In the field of surgery, augmented reality began to be explored as a tool to enhance surgical visualization and navigation. Surgeons could wear AR glasses or use headsets that projected virtual images onto the real-world surgical field. This allowed for better visualization of anatomical structures, identification of critical structures, and improved surgical planning.
The Current State of Augmented Reality in Surgery
Today, augmented reality has become an integral part of the modern operating room. Surgeons can use AR to overlay patient-specific data, such as preoperative imaging, onto the surgical field in real-time. This enables them to precisely locate tumors, navigate complex anatomical structures, and perform procedures with greater accuracy.
AR also has the potential to enhance surgical education and training. Medical students and residents can use AR simulations to practice procedures in a realistic virtual environment, allowing for repetitive practice and skill development without the need for live patients.
Furthermore, AR can facilitate remote collaboration and consultation. Surgeons can share their augmented view with colleagues in different locations, enabling real-time guidance and support during complex surgeries.
While augmented reality in surgery has come a long way, there are still challenges to overcome. The technology needs to become more seamless and intuitive, with improved image quality and reduced latency. Additionally, issues regarding data privacy and security must be addressed to ensure patient confidentiality.
Despite these challenges, the future of surgery looks promising with augmented reality at its forefront. As technology continues to advance, we can expect further integration of AR into surgical practice, leading to improved patient outcomes and revolutionizing the operating room as we know it.
FAQs about the Future of Surgery: Augmented Reality Revolutionizes the Operating Room
1. What is augmented reality (AR) in the context of surgery?
Augmented reality is a technology that overlays virtual objects or information onto the real world. In surgery, AR involves the use of special headsets or displays that allow surgeons to see digital images, such as medical scans or real-time data, superimposed onto the patient’s body during an operation.
2. How does augmented reality benefit surgeons?
AR provides surgeons with real-time, contextual information during procedures. It can display patient-specific anatomical structures, highlight critical blood vessels or nerves, and show the position of surgical instruments. This enhances surgical precision, reduces errors, and improves patient outcomes.
3. Can you give some examples of how augmented reality is being used in surgery?
Sure! Augmented reality is being used in various surgical specialties. For instance, in neurosurgery, AR can help surgeons navigate complex brain structures with greater accuracy. In orthopedic surgery, it can aid in aligning implants and guide incisions. Additionally, AR is being explored for training purposes, allowing surgeons to practice procedures in a virtual environment.
4. Is augmented reality only used during open surgeries, or can it be applied to minimally invasive procedures as well?
While AR is more commonly associated with open surgeries, it is also being adapted for minimally invasive procedures. For example, it can assist laparoscopic surgeons by providing 3D visualizations of internal organs and guiding instrument placement. This technology has the potential to revolutionize the way minimally invasive surgeries are performed.
5. Are there any risks or limitations associated with using augmented reality in surgery?
Like any emerging technology, there are challenges to address. One concern is the potential for visual distractions or information overload for surgeons. Another challenge is the need for accurate registration of virtual objects onto the patient’s anatomy. Additionally, the cost of implementing AR systems can be a barrier for some healthcare institutions.
6. How accessible is augmented reality technology for hospitals and surgical teams?
Augmented reality technology is becoming more accessible as it evolves. While early adopters in research institutions and large hospitals have been at the forefront of its integration, the costs are expected to decrease over time. As the technology matures, it is likely to become more widely available to hospitals and surgical teams of varying sizes.
7. What impact does augmented reality have on patient outcomes and recovery?
Augmented reality has the potential to improve patient outcomes by reducing surgical complications and improving surgical precision. By providing surgeons with real-time guidance and critical information, AR can enhance the accuracy and safety of procedures. This can lead to shorter recovery times, reduced post-operative pain, and improved overall patient satisfaction.
8. Are there any ethical considerations associated with using augmented reality in surgery?
As with any technological advancement, there are ethical considerations to be mindful of. Patient privacy and data security are paramount when using AR systems that incorporate patient-specific information. Additionally, surgeons must be properly trained and certified to use augmented reality technology to ensure its safe and effective implementation.
9. What does the future hold for augmented reality in surgery?
The future of augmented reality in surgery is promising. As the technology continues to advance, we can expect more sophisticated and user-friendly AR systems. This may include features such as real-time feedback, integration with artificial intelligence, and remote collaboration capabilities. Augmented reality has the potential to become a standard tool in the operating room, benefiting both surgeons and patients.
10. How long until augmented reality becomes a widespread practice in surgery?
The widespread adoption of augmented reality in surgery will depend on several factors, including technological advancements, cost-effectiveness, and regulatory considerations. While it may take some time for AR to become a standard practice, the growing interest and ongoing research in this field suggest that it will become increasingly common in the coming years.
1. Stay Informed
Keeping up with the latest advancements in augmented reality (AR) technology and its applications in surgery is essential. Follow reputable medical journals, technology news websites, and social media accounts to stay informed about the latest developments.
2. Embrace Lifelong Learning
AR technology is continuously evolving, so it’s important to embrace lifelong learning. Attend conferences, workshops, and webinars to enhance your understanding of AR in surgery. Engage with experts in the field and be open to expanding your knowledge.
3. Explore Virtual Reality (VR) Simulations
VR simulations can provide a safe and immersive environment to practice surgical procedures. Look for VR platforms or applications that offer simulated surgeries. These simulations can help you develop and refine your skills without the risks associated with real patients.
4. Collaborate with Colleagues
Collaboration is key when it comes to adopting new technologies. Engage with your colleagues, both within and outside your specialty, to discuss the potential applications of AR in your daily practice. Share experiences, insights, and best practices to collectively explore the benefits of AR in surgery.
5. Seek Training Opportunities
As AR becomes more prevalent in the operating room, seek out training opportunities to familiarize yourself with the technology. Look for courses or workshops that specifically focus on AR in surgery. Hands-on training will help you become more comfortable and proficient in using AR tools.
6. Understand Patient Education
AR can play a significant role in patient education. Familiarize yourself with AR applications that can help explain surgical procedures to patients in a more visual and interactive manner. Use these tools to enhance patient understanding and improve shared decision-making.
7. Stay Ethical and Responsible
While AR technology can revolutionize surgery, it’s important to maintain ethical and responsible practices. Ensure that patient privacy and confidentiality are protected when using AR tools. Adhere to professional guidelines and regulations to ensure the responsible use of AR in the operating room.
8. Advocate for AR Adoption
Be an advocate for the adoption of AR technology in your workplace. Educate your colleagues, administrators, and decision-makers about the potential benefits of AR in surgery. Present evidence-based arguments and share success stories to encourage the integration of AR tools into daily practice.
9. Embrace Interdisciplinary Collaboration
AR technology requires collaboration not only within the medical field but also with experts from other disciplines. Engage with engineers, computer scientists, and developers to explore new possibilities and push the boundaries of AR in surgery. Embracing interdisciplinary collaboration can lead to innovative solutions and advancements.
10. Stay Adaptable
AR technology is still evolving, and its full potential is yet to be realized. Stay adaptable and open to new developments. As more applications and tools emerge, be willing to adapt your practice and embrace the changes that AR brings to the operating room.
Concept 1: Augmented Reality in Surgery
Augmented Reality (AR) is a technology that combines virtual elements with the real world. In the context of surgery, AR can be used to provide surgeons with additional information and guidance during procedures. Imagine wearing a special headset that allows you to see virtual images overlaid onto the patient’s body. These virtual images can include things like 3D models of organs, blood vessels, or tumors. By using AR, surgeons can have a better understanding of the patient’s anatomy and make more precise incisions or placements of medical devices.
Concept 2: Surgical Navigation
Surgical navigation is a technique that helps surgeons navigate through complex anatomical structures during a procedure. Traditionally, surgeons rely on their knowledge and experience to guide them. However, with the help of augmented reality, surgical navigation becomes more accurate and efficient. By using AR, surgeons can see real-time images of the patient’s internal structures, such as bones or blood vessels, overlaid onto their field of view. This allows them to better visualize the patient’s anatomy and make more informed decisions during surgery. For example, if a surgeon needs to place a screw in a specific location in a bone, AR can help them precisely locate that spot.
Concept 3: Training and Education
Augmented reality is also transforming the way surgeons are trained and educated. In the past, surgical trainees would learn by observing surgeries or practicing on cadavers. While these methods are still valuable, AR offers a new way to enhance surgical education. With AR, trainees can wear a headset and see virtual surgical procedures overlaid onto a physical model or a real patient. This allows them to practice their skills in a realistic and controlled environment. They can also receive real-time feedback and guidance from experienced surgeons, who can use AR to annotate or highlight important structures during the training session. This immersive and interactive learning experience can help trainees develop their surgical skills more effectively and efficiently.
Common Misconceptions about the Future of Surgery: Augmented Reality Revolutionizes the Operating Room
Misconception 1: Augmented reality in surgery is just a gimmick
One common misconception about the future of surgery is that augmented reality (AR) is merely a gimmick or a fancy technology without any real benefits. However, this is far from the truth. Augmented reality has the potential to revolutionize the operating room by providing surgeons with real-time, interactive, and immersive information during surgical procedures.
AR overlays digital information onto the surgeon’s view of the patient, enhancing their perception and understanding of the anatomy. This can help in various ways, such as improving accuracy, reducing errors, and enhancing surgical planning. For example, AR can provide surgeons with preoperative imaging, allowing them to visualize the patient’s anatomy in 3D before making any incisions.
Furthermore, AR can assist in intraoperative navigation, guiding surgeons to the precise location of tumors or other structures of interest. This can be particularly beneficial in complex surgeries where anatomical landmarks may be difficult to identify. By providing real-time guidance, AR can help surgeons perform procedures with greater precision and confidence.
Misconception 2: Augmented reality is only useful in complex surgeries
Another misconception is that augmented reality is only useful in complex surgeries, and it has limited applications in routine procedures. While AR certainly has significant potential in complex surgeries, its benefits extend beyond just the most intricate cases.
Even in routine procedures, AR can enhance surgical precision and efficiency. For example, in orthopedic surgeries, AR can assist in aligning implants with the patient’s anatomy, reducing the risk of malpositioning. In minimally invasive procedures, AR can provide surgeons with real-time feedback, ensuring that they are navigating the instruments correctly and avoiding vital structures.
Moreover, AR can also be valuable in training and education. Medical students and residents can benefit from the immersive and interactive nature of AR, allowing them to practice surgical techniques and learn anatomy in a realistic virtual environment. This can help bridge the gap between theory and practice, ultimately improving the quality of surgical training.
Misconception 3: Augmented reality is not safe for patients
There is a concern that incorporating augmented reality into the operating room may compromise patient safety. However, this is a misconception that overlooks the rigorous development and testing processes that AR technologies undergo before being implemented in surgical settings.
AR systems are designed with patient safety in mind. They undergo extensive validation and verification processes to ensure their accuracy and reliability. The technology is continuously refined and improved based on feedback from surgeons and patients.
Furthermore, AR can actually enhance patient safety by reducing the risk of errors and complications. By providing surgeons with real-time feedback and guidance, AR can help prevent accidental damage to vital structures and improve surgical outcomes. It can also assist in preoperative planning, allowing surgeons to anticipate potential challenges and develop strategies to mitigate them.
It is important to note that augmented reality is not meant to replace the surgeon’s expertise but rather to augment their capabilities. Surgeons will always remain in control and make the final decisions during surgical procedures.
Augmented reality is not just a gimmick, but a technology with immense potential to revolutionize the operating room. It can enhance surgical precision, reduce errors, and improve patient outcomes. Augmented reality is not limited to complex surgeries but can benefit routine procedures as well. Patient safety is a top priority, and AR technologies undergo rigorous testing to ensure their reliability and accuracy. It is crucial to dispel these misconceptions and embrace the potential of augmented reality in shaping the future of surgery.
In conclusion, augmented reality has the potential to revolutionize the operating room and transform the way surgeries are performed. This technology provides surgeons with real-time, interactive information that enhances their precision and decision-making abilities. By overlaying digital images onto the patient’s anatomy, surgeons can visualize complex structures and navigate through delicate areas with greater confidence and accuracy. Additionally, augmented reality can improve communication and collaboration among surgical teams, allowing for more efficient and effective procedures.
However, there are still challenges that need to be addressed before augmented reality becomes a standard tool in the operating room. Issues such as the integration of multiple data sources, the development of user-friendly interfaces, and the need for robust and reliable hardware must be overcome. Furthermore, ethical considerations regarding patient privacy and the potential for information overload need to be carefully examined. Nevertheless, as technology continues to advance and these challenges are addressed, augmented reality has the potential to transform surgery and improve patient outcomes in ways we have never imagined.